Water pollution
There’s no doubt that water is important. Water covers 70.9% of the earth’s surface, and is vital for all known forms of life which depend on water. As such testing for water pollution to ensure it is fit for use is important!
Life on earth has been distressed by the growing number of ecological problems that are mostly caused by humans themselves (factories, sewage treatment plants, underground mines, oil wells, oil tankers and agriculture, acid deposition from the air, traffic, pollutants that are spread through rivers or pollutants that enter the water through groundwater). Water pollution takes place when pollutants are released directly or indirectly into bodies of water without sufficient treatment to eliminate damaging compounds.
Water pollution
- affects drinking water, rivers, lakes and oceans all over the world. This consequently harms human health and the natural environment.
- is the second most imperative environmental concern along with air pollution.
- is any change or modification in the chemical, physical or biological quality of water that has a harmful effect on any living thing that drinks or uses or lives (in) it.
- may not damage our health immediately but can be harmful after long term exposure.
- can also make water unsuited for the desired use.
- involves the contamination of surface waters and groundwater which may set off a series of diseases referred to as water pollution diseases.
Water pollution can occur in many ways. There are two main sources of contamination – bacterial and chemical.
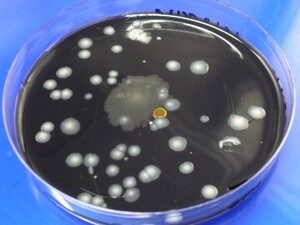
Bacterial contamination is usually measured by the fecal coliform levels in the water. Fecal coliform is an indicator organism; it is easily measured and can signal the presence of other harmful bacteria in water. This sort of bacterial contamination can occur as a result of improper water treatment (for example, not chlorinating water from a wastewater treatment plant properly), as a result of rotten or corroded piping allowing bacterial growth in pipes, or as a result of poor water storage.
Polluted water is unfit, unhealthy, and dangerous for drinking and for other consumption processes. It is also not suitable for agricultural and industrial assistance. This water pollution is harmful to human beings, plants, animals, fish and birds. Contaminated water also houses and contains viruses, bacteria, intestinal parasites, and other harmful microorganisms, which can originate waterborne diseases such as diarrhea, dysentery, and typhoid.
MBL Laboratories can help you to determine the level of bacterial contamination in the water. Our laboratory specializes in bacterial analysis of waters – wastewaters, lakes, rivers, ponds, storm waters, ground waters. If you need to determine the level of fecal coliforms, E.coli, total coliforms, heterotrophic plate count, Legionella or other type of bacteria in the water call our Mississauga office at 905-290-9101 or our Burnaby office at 604-435-6555.