Legionella pneumophila is a Gram negative, aerobic bacteria that is characterized as an opportunistic pathogen. It is the cause of Legionnaires’ Disease, a severe form of pneumonia and, it is the cause of Pontiac fever, a non-pneumonic form of L. pneumophila infection. Legionella spp.’s mode of transmission is through aerosols or aspiration of contaminated water.
The Public Health Agency of Canada has posted an informative pathogen safety data sheet on Legionella pneumophila which can be viewed at:
http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/legionella-eng.php
Legionella spp. can be isolated from numerous places. Samples should be transported to the lab immediately and kept cool in sterile containers. Chlorinated water should be treated with sodium thiosulfate to neutralize the chlorine. Water samples should be brought to the lab ideally within a few hours of sampling and should be stored at room temperature (20 + 5°C) in the dark.
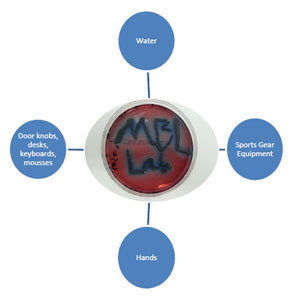
Examples of sampling areas:
A. Potable water (1 L in sterile container):
– Municipal water (hot water tanks), hoses, well water, faucets, water fountains, sinks, respiratory therapy equipment, showers, eye washers, bottled water or cooler water systems.
Note: Collect 2 water samples from shower heads, tap water faucets, respiratory therapy equipment, water fountains, etc. First a pre-flush or first draw sample by draining the first 1 L of water from the faucets or flush drains into a bottle. Allow the water to run for approximately 1 minute and collect the second draw of 1 L of water.
B. Non-potable water (250 mL in sterile container):
– Cooling towers, humidifiers, decorative fountains, HVAC systems, dire sprinkler systems, storage tanks, basin water, hot tubs, surface water from reservoirs, misters.
C. Swabs:
– Faucet aerators, condensate pan, shower heads, condenser coils.
D. Bulk samples:
– Sludge from the bottom of a condensate pan scraped off a cooling coil.
E. Legionella Air Sampling requires the following which can be provided by MBL Inc.:
- Latex gloves
- 70% Isopropyl alcohol to sterilize sampler after every other sample
- SKC QuickTake 30 pump with Andersen N-6 single stage Impactor
- BCYE (Buffered Charcoal Yeast Extract) agar
Interpretation of Legionella results:
Table 1. The following chart can be used as a guideline for interpretation of Legionella spp. results received from the laboratory.
| Action (see below)
1 2 |
Cooling tower
100 1,000 |
Domestic water
10 100 |
Humidifier
1 10 |
Action 1: Prompt cleaning and/or biocide treatment of the system.
Action 2: Immediate cleaning and/or biocide treatment. Take prompt steps to prevent employee exposure.
(Source: From OSHA Technical Manual (Section III: Chapter 7, Legionnaires’ Disease), which was adapted from George K. Morris, PhD, and Brian G. Shelton, Pathcon Technical Bulletin 1.3, Legionella in Environmental Samples: Hazard Analysis and Suggested Remedial Actions, June 1991)
For more information on Legionella testing or to find out about our other bacteria and mold testing services, please contact Mold & Bacteria Consulting Laboratories, call our Ontario, Mississauga Office at 905-290-9101 or the British Columbia, Burnaby Office at 604-435-6555.